Cataract surgery is the most common operation done as an outpatient procedure in the NHS. Mr Adams and Miss Maling co-lead the Buckinghamshire Healthcare Trust Cataract Service which this year 2021 is the most productive Cataract Service in the country. Mr Adams and Miss Maling both have training in all aspects of cataract surgery including multifocal lenses, extended range of focus lenses, mono-focal lenses and paediatric cataract surgery.
Mr Adams and Miss Maling have developed a pathway for high volume low complexity cataract surgery which has now been adopted by many centres in the UK and are delighted to be able to offer bespoke cataract surgery for all their patients depending on their visual outcome needs.
All cataract patients undergo a full pre-operative assessment including imaging of their retina with a full pre-operative refractive plan such that the outcome of cataract surgery is concluded before proceeding with surgery.
Both Mr Adams and Miss Maling are happy to carry out unilateral, sequential and/or bilateral cataracts surgery under local anaesthetic, sedation and/or general anaesthesia. Within the Sight Surgery complex, local anaesthesia is available. General anaesthetic and sedation procedures would need to be carried in the hospital setting.
What is a cataract?
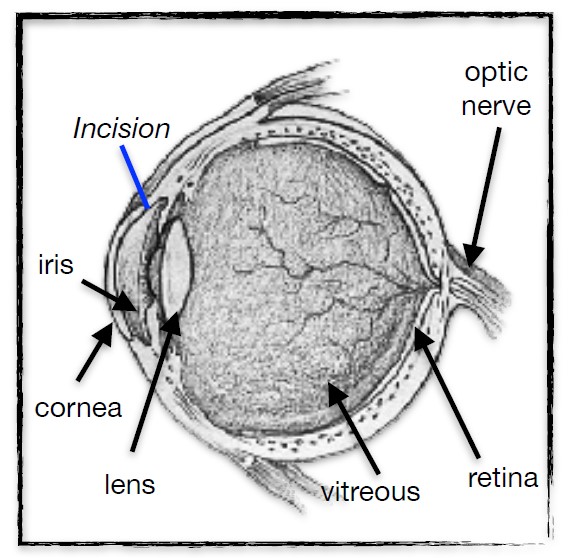
Cataract is the name given to a clouding of the natural lens in the eye. The lens sits behind the iris – the coloured part of the eye – and focuses light onto the retina.
What causes a cataract?
The commonest cause is simply ageing: when we are born the lens is clear; but with time it gradually becomes opaque. Some medical conditions, and certain medicines such as high-dose oral steroids, can cause a cataract to form earlier, as can some eye operations. There are genetic conditions which may result in cataracts developing very early in life, but these are uncommon.
What problems does a cataract cause?
This depends on the type of cataract, and its location within the lens: glare, dazzle from oncoming headlights, a loss of clarity, or loss of brightness are all common symptoms. Cataracts cause a gradual, progressive, drop in vision so if your visual symptoms fluctuate from minute to minute, they are unlikely to be due to cataract.
How is a cataract removed?
Cataract surgery is normally performed under local anaesthetic, and takes around twenty minutes. A small self-sealing incision is made in the cornea and the capsule containing the lens is opened. Ultrasound energy then breaks the lens up into very small particles, and fluid aspiration is used to remove these fragments, leaving the lens capsule clear and empty. The replacement intraocular lens (IOL) is injected through the corneal incision and into the empty lens capsule where it slowly unfolds and is carefully positioned. At the end of the operation antibiotics are administered and usually no stitches are needed.
What are the benefits of cataract surgery?
Removing the cataract restores clarity to the vision, optimises light transmission to the retina, and often improves colour perception. The IOL is made from a flexible acrylic, and lasts a lifetime.
Will I need glasses after cataract surgery?
This depends on which type of IOL is implanted. Before surgery, the eye is carefully measured and the IOL strength is calculated to leave the eye focussed for a particular distance, effectively incorporating the spectacle prescription into the IOL. Most people choose an IOL which will leave the eye naturally focussed for distance, just needing glasses to read fine print. Occasionally, people who have been short-sighted (‘myopic’) for their whole life, and who have been used to taking their glasses off to read, prefer to stay that way. In addition there are multi-focal lenses available which aim to provide both distance and near vision without glasses. These lenses can result in a subtle compromise of contrast sensitivity, so it’s important to discuss this fully before deciding on a lens.
How soon can I get back to normal after surgery?
Gentle activity such as walking is fine; watching TV, reading, or working on a computer will not do any harm. For the first week it is sensible to avoid strenuous activities, and avoid rubbing or knocking the eye. For the first month it is best to avoid swimming or contact sports. Most people can return to work after a few days; but if your job is physically strenuous or involves working in dusty or hazardous environments, plan for two weeks off work.
How soon can I drive?
The Driver and Vehicle Licensing Agency (DVLA) requires you to be able to read a number plate at 20 metres (22 yards), with both eyes open. For most people, this means a waiting a few days until the eye has settled down; but if you have a high spectacle prescription, or an imbalance between the eyes, you may need longer.
When can I get new glasses?
If you need glasses after surgery, it is sensible to wait six weeks before seeing your optometrist. This gives the eye time to heal fully, and ensures that your optometrist can get an accurate result. Off-the-peg +2.50 or +3.00 reading glasses, readily available in most supermarkets, are a safe temporary measure.
What are the risks of cataract surgery?
Cataract surgery is very safe, and the risk of complications is very low. There are three time-points when problems may arise. The first point is during surgery itself: if the lens capsule breaks during the operation, an extra step is required to clear any strands of vitreous gel which may have come forward from the back part of the eye. The risk of this is approximately 1 in 300. The final visual outcome is usually just as good, but occasionally the insertion of the IOL needs to be deferred if portions of cataract have fallen back into the vitreous cavity.
Secondly, in the first few days after surgery, the eye normally becomes more comfortable and the vision improves. If, instead, the eye becomes more uncomfortable, or the quality of vision drops, this may be a sign of an infection inside the eye (endophthalmitis). Such an infection is treated as an emergency; but if the bacteria have damaged the retina, then even with treatment the final vision may be worse than it was before cataract surgery. Fortunately the risk of endophthalmitis is extremely small, and with newer techniques has become as low as 1 in 3000. Thirdly, three or four weeks after surgery, a small proportion of people may develop swelling in the central retina (cystoid macular oedema or CMO), and notice a drop in the quality of vision. CMO usually responds well to anti-inflammatory eye-drops; it is
more common in diabetics, who are therefore routinely given this extra medication as part of their post-operative treatment.
In the longer term, one in ten eyes may develop ‘posterior capsule opacification’ (PCO). This develops in the months or years following surgery, and occurs when the back part of the lens capsule becomes thickened and cloudy, scattering the light and reducing the quality of vision. PCO can be treated with a laser procedure (YAG laser capsulotomy) to break up the thickened capsule and restore the vision. YAG laser procedures are performed in the outpatient clinic, and take just a few minutes.
Recovering from cataract surgery
Depending on the type of anaesthetic you have had, it may take a couple of hours for feeling to return to the eye, and the vision may be blurry until the next day. The plastic shield over your eye can be removed next day: please wear it at night for the first week to prevent accidentally rubbing the eye when asleep. Take it easy for the first few days after surgery.
The following are normal side-effects:
• mild pain or grittiness in and around your eye
• an itchy or sticky eye
• blurred vision
• very slight headache
• bruising of the skin around the eye
• discomfort when looking at bright lights
These should improve within a few days, and over-the-counter painkillers – such as paracetamol or ibuprofen – will help; sunglasses will alleviate light-sensitivity.
Post-operative eyedrops
The drops you have been given are important to protect the eye from infection and promote healing: please start using these the morning after surgery:
Maxidex: one drop 4 times a day for 2 weeks, then twice a day for 2 weeks
Acular: one drop 4 times a day for 2 weeks, then twice a day for 2 weeks
Chloramphenicol: one drop 4 times a day for 2 weeks, then stop.
When to seek medical advice
Seek medical advice as soon as possible if you experience:
• a throbbing or severe pain in or around your eye
• a severe frontal headache
• a sudden deterioration or loss of vision
• increasing redness in your eye
• the sudden appearance of black dots, specks or streaks in your field of vision (floaters) or flashes of light in your eye
These problems may be a sign of a complication of cataract surgery.